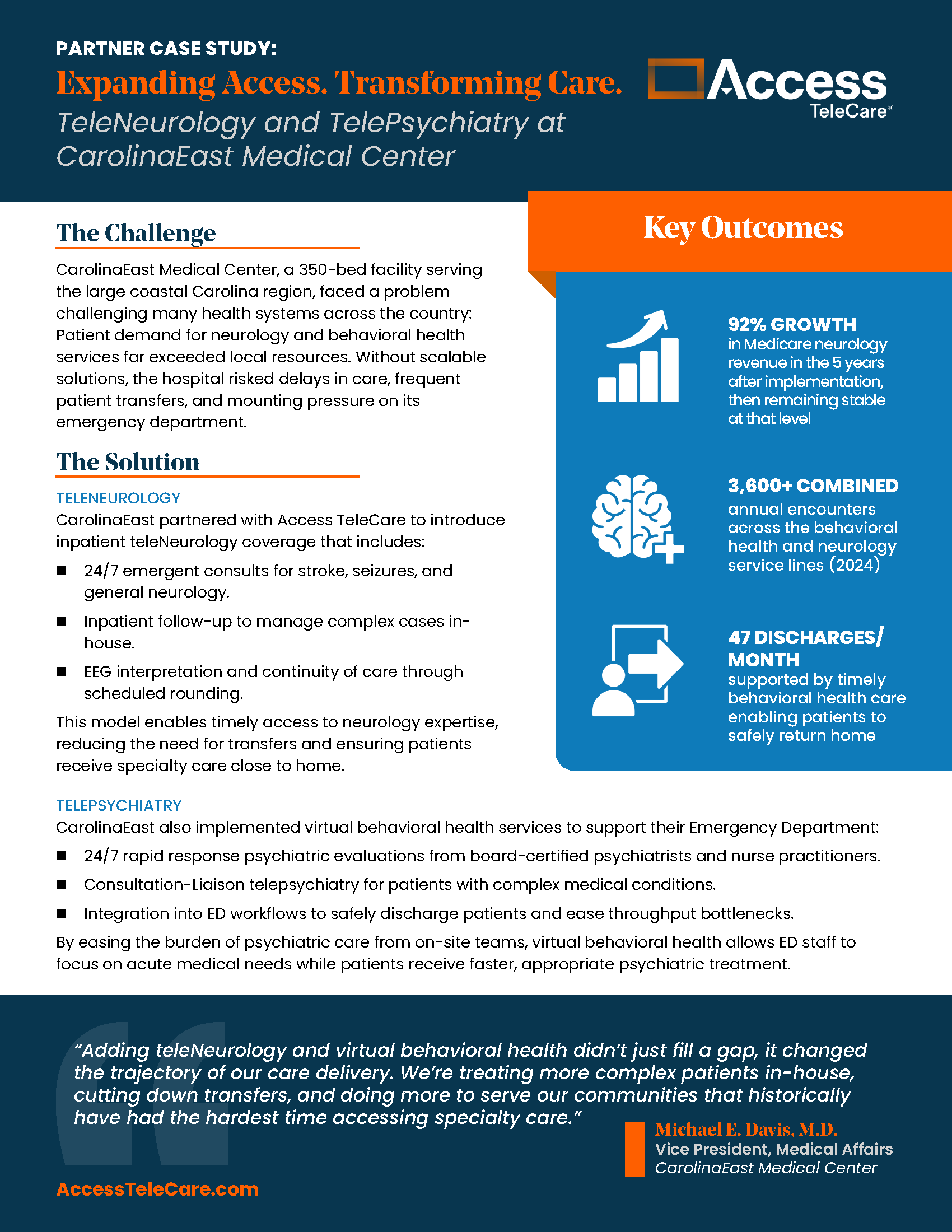
Expanding Access. Transforming Care. TeleNeurology and TelePsychiatry at CarolinaEast Medical Center
Access TeleCare Case Study
When specialty care is available close to home, communities benefit. At CarolinaEast Medical Center, Access TeleCare’s teleNeurology and telePsychiatry programs are helping patients get timely treatment, reducing transfers, and easing pressures on the emergency department.
Hospital Telemedicine Solutions
The Challenge:
CarolinaEast Medical Center, a 350-bed facility serving the large coastal Carolina region, faced a problem challenging many health systems across the country: Patient demand for neurology and behavioral health services far exceeded local resources. Without scalable solutions, the hospital risked delays in care, frequent patient transfers, and mounting pressure on its emergency department.
The Solution:
TELENEUROLOGY
CarolinaEast partnered with Access TeleCare to introduce inpatient teleNeurology coverage that includes:
- 24/7 emergent consults for stroke, seizures, and general neurology.
- Inpatient follow-up to manage complex cases in-house.
- EEG interpretation and continuity of care through scheduled rounding.
This model enables timely access to neurology expertise, reducing the need for transfers and ensuring patients receive specialty care close to home.
TELEPSYCHIATRY
CarolinaEast also implemented virtual behavioral health services to support their Emergency Department:
- 24/7 rapid response psychiatric evaluations from board-certified psychiatrists and nurse practitioners.
- Consultation-Liaison telepsychiatry for patients with complex medical conditions.
- Integration into ED workflows to safely discharge patients and ease throughput bottlenecks.
By easing the burden of psychiatric care from on-site teams, virtual behavioral health allows ED staff to focus on acute medical needs while patients receive faster, appropriate psychiatric treatment.
“Adding teleNeurology and virtual behavioral health didn’t just fill a gap, it changed the trajectory of our care delivery. We’re treating more complex patients in-house, cutting down transfers, and doing more to serve our communities that historically have had the hardest time accessing specialty care.”
Michael E. Davis, M.D., Vice President, Medical Affairs
CarolinaEast Medical Center
TeleNeurology solutions include:
TelePsychiatry solutions include:
Telemedicine Results
3,600+ virtual encounters each year
3,600+ virtual encounters each year
3,600+ combined annual encounters across the behavioral health and neurology service lines (2024)92% growth in neurology Medicare revenue
92% growth in neurology Medicare revenue
92% growth in Medicare neurology revenue in the 5 years after implementation, then remaining stable at that level.47 safe discharges/month supported by telePsychiatry
47 safe discharges/month supported by telePsychiatry
47 discharges/month supported by timely behavioral health care enabling patients to safely return homeTelemedicine Outcomes
By deploying both teleNeurology and telePsychiatry, CarolinaEast has been able to fundamentally shift how it delivers specialty care. With over 3,600 encounters occurring annually via telemedicine, more patients are getting access to high-quality specialty care while also helping the hospital financially.
For example, CarolinaEast experienced a 92% increase in Neurology Medicare revenue in the five years after implementation, with revenue remaining stable at that level in the years following. Patients who once would have been transferred out for treatment are now staying closer to home, receiving the expertise they need without the disruption and risk of leaving the community. This reduction in transfers has strengthened continuity of care while reinforcing the hospital’s role as the region’s trusted provider.