What is Acute Care Telemedicine? Expanding Access to Urgent Medical Expertise
What is Acute Care Telemedicine?
Acute care telemedicine is a consultation in a hospital or other emergency setting for urgent medical cases with a remote physician specialist, such as a teleNeurologist, telePsychiatrist, or teleIntensivist.
Acute care is the short-term treatment for a sudden onset of an illness, urgent medical condition, or severe injury. Acute care telemedicine is typically used in hospitals and other emergency settings. Care for acute health issues is very different than routine, chronic, or long-term care concerns, which is why acute care telemedicine is very different than direct-to-consumer telemedicine.
What are some examples of acute care telemedicine ?
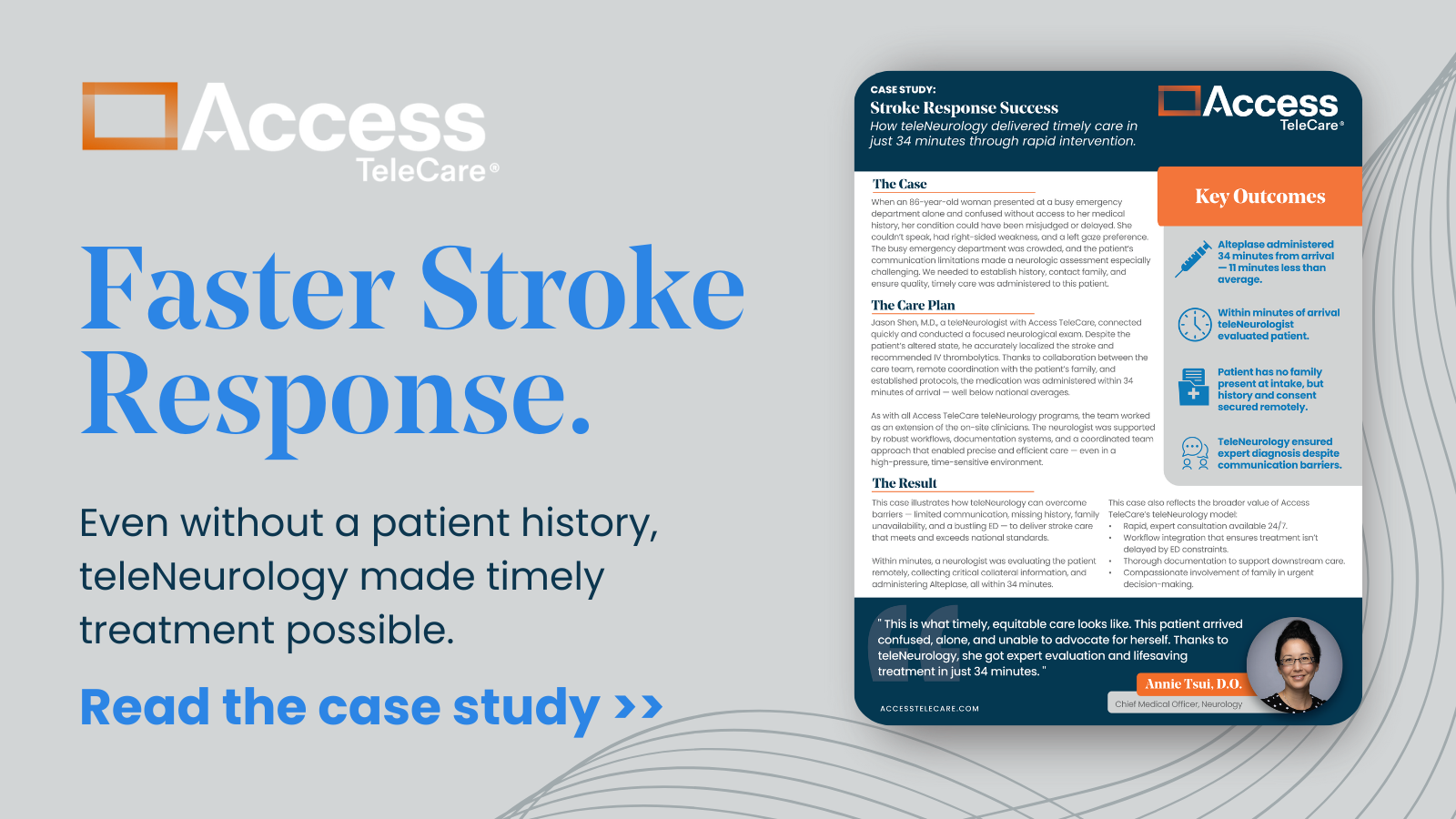
Telestroke is one example of acute care telemedicine. Strokes are one of the leading causes for visits to the emergency room. A hospital with a teleNeurology program can call a remote neurologist to consult on the patient within minutes of getting CT images of suspected strokes. This neurologist meets with the patient and their family and recommends a course of action, which can include administration of a clot-busting drug, which is sometimes referred to as tPA, or endovascular surgery to remove a clot.
Another example is telePsychiatry. One in eight patients in an Emergency Department has a mental health or substance abuse issue. It is common for these patients to arrive at the emergency department in need of care. But EDs are built for medical emergencies, not psychiatric ones. Mental health patients often wait for hours or even days to see a psychiatrist who can help determine whether they need to be admitted or discharged for outpatient care. A telePsychiatry offering helps patients receive the mental health care they need, fast, while improving throughput in the facility.
Amazingly, even the ICU can be served by a remote specialist called an intensivist. TeleIntensivists can provide on-demand critical care expertise and support at the point of care anywhere in the health system and can be engaged clinically within minutes to evaluate the patient’s status and needs, just as any onsite ICU physician would manage their patient population. TeleICU services and solutions provide complete 24/7 coverage by board-certified intensivists and enhanced clinical decision support.
More From Access TeleCare
See the difference clinically led and clinically driven telemedicine programs can make for your patients.
What are the benefits of Acute Care Telemedicine ?
Acute care telemedicine can:
- Help hospitals and clinics expand specialty acute care delivery, especially for specialists in short supply, such as neurologists, psychiatrists, and intensivists. Some hospitals must transfer all but the most basic cases because they don’t have the specialists needed to keep patients local. And, some smaller hospitals are bypassed by EMS entirely because they are not certified for stroke care. And many hospitals have had to close their ICUs altogether because of a lack of intensivists on staff.
- Extend care to those who are admitted or need home monitoring after hospitalization. Instead of physicians or nurses traveling to skilled nursing facilities or making home visits, they can see patients via videoconference. Patients don’t have to risk weather or traffic for office visits for routine or follow up care.
- Provide better mental health care in emergency rooms. Psychiatrists are required in many states to evaluate patients for the risk of harming themselves or others before they can be admitted or discharged for outpatient treatment. Many patients wait hours, if not days, to be seen by a psychiatrist; acute care telemedicine helps provide that care much faster.
What is driving the increase in utilization of acute care telemedicine ?
Physician Shortages
The U.S. will experience a shortage of as many as 60,300 specialty physicians by 2025, mainly due to population growth, aging, and the fact that more than two in five active physicians will be at retirement age within the next decade. Rural communities will have it worse—with almost a quarter of Americans living in rural areas and only 9% of physicians practicing there.
Many hospitals have telemedicine capabilities now. Smaller hospitals are likely to have processes in place to deal with specific uses where they have the biggest need for specialists that they don’t have on staff. Two areas that are the most common for small hospitals are acute stroke care and emergency psychiatry.
Aging population
Physician shortages and the uneven national distribution of specialists are exacerbated by an aging population, which will result in higher patient volumes, increasing demand. By 2030, every Baby Boomer will be age 65 or older. As the population ages, chronic medical conditions will increase significantly. The need to expand clinical capacity can be met with deploying our scarce resources via telemedicine in a cost-effective and efficient manner.
Pandemic
The increase of telemedicine visits during the pandemic is now well-documented. Telemedicine protects not just patients, but also physicians, from the risk of infection. Telemedicine can help with keeping non-urgent cases out of hospitals, too, freeing up resources, protective gear, and space for critically-ill patients.
Regulatory and Compliance Issues
The ever-changing regulatory and compliance landscape can create profound financial pressure for hospitals and directly impact their bottom line. Telemedicine is emerging as a solution to create additional clinical capacity, improve clinical quality, and drive operational efficiencies—creating a path to improved profitability for struggling healthcare providers.
Conclusion
Acute care telemedicine gives hospitals the ability to deliver qualified care to any location in minutes. It can also enable coordinated care for patients recovering at home or in rehab facilities or nursing homes, eliminating the need for patient travel to hospitals. Not only do patients benefit, but physicians can treat more patients and be on call to consult remotely at multiple hospitals.