There’s hardly a single hospital anywhere in the country that hasn’t experienced difficulties finding an appropriate behavioral health placement for a patient with a mental health emergency. The consequences are increased ED wait times for all patients, care delays, loss of revenue, and degraded patient satisfaction.
The problem of ED boarding is complex, with a lack of available psychiatrists, hospital overcrowding, and a rising demand for care all contributing to the issue, and there is no single answer. But, access to reliable, consistent, high-quality psychiatrists through telemedicine is a proven solution.
Behavioral Health Telemedicine Advantages for Patients
With the American College of Emergency Physicians calling ED boarding a “public health emergency,” the group calls out ED boarding of psychiatric patients in particular. These patients wait three times longer, on average, than medical patients for appropriate placement. Stories of patients of all ages waiting days, weeks, and even months for a mental health specialist to see them are common.
“When patients are experiencing an acute psychiatric crisis, being stuck in an emergency department waiting room or hallway can be overstimulating and one of the worst places for them to be,” says Access TeleCare’s chief of psychiatry, John Kenny, M.D. “We’re able to get more patients the care they need faster by evaluating patients within a few hours of them entering the hospital, not days.”
The consequences for patients are severe. Delays in care. Patient decompensation. Poorer outcomes. Patients deciding to leave the ED without receiving care and deciding not to seek out emergency care in the first place because of concerns about long wait times.
Behavioral Health Telemedicine Advantages for Hospitals
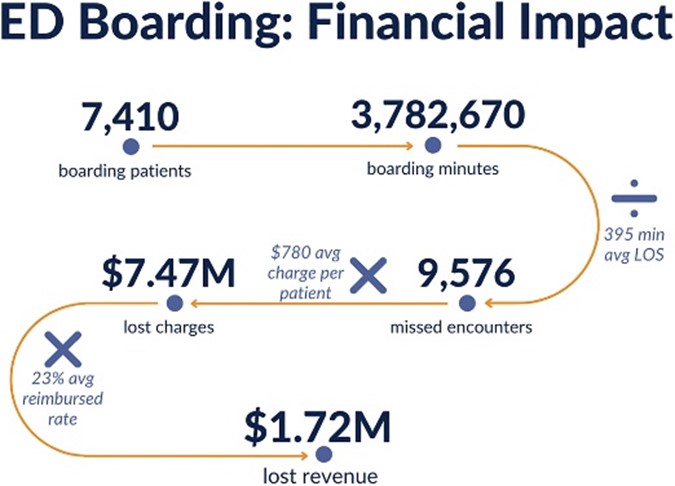
For hospitals, the consequences are financial, operational, and clinical. Staff burnout is higher. Financial losses are higher. Operational inefficiencies are greater.
One analysis estimated the annual financial loss at one large academic hospital of patient boarding to exceed $1.7 million.
While the nationwide shortage of psychiatrists makes it impossible for all hospitals to have available on-site 24/7 psychiatric coverage for their ED, telemedicine offers an almost immediate solution. With psychiatrists and psychiatric mental health nurse practitioners available through telemedicine, hospital ED staff have a trusted source of psychiatric expertise available 24/7, as needed, to diagnose, stabilize, and transfer patients in crisis while reducing ED wait times for all patients.
The positive impacts for patients, hospitals, and staff are significant:
- A 1-hour reduction in ED boarding time yields additional daily revenue of $9,693 to $13,298 just from retaining patients who would have left without being seen and patients who would have been diverted via ambulance to another facility.
- A 30-minute reduction in ED boarding time creates additional capacity to see 8.7 to 36 more patients per day, with a potential annual revenue increase of $2.7 to $3.9 million.
- Patient satisfaction with wait times increases 20 percent with reduced ED wait times.
- By increasing ED throughput and efficiencies, one hospital reduced its “door-to-provider” time from 70 minutes to just over 10 minutes and increased its patient satisfaction scores from 8 percent to nearly 80 percent.
Access TeleCare has deployed virtual behavioral health programs in hospitals across the country for more than two decades, from the largest health systems to the smallest critical access hospitals.
Read more here and contact us to explore how we can customize a solution for your hospital.