What is teleMentalHealth ?
TeleMentalHealth, also known as telePsychiatry and teleBehavioralHealth, is virtual care for mental health and substance abuse patients.
The treatment of mental health patients by a remote clinician (psychiatrist, psychologist, licensed clinical social worker, etc.) using telecommunications technology like videoconferencing makes it possible for patients to seek ongoing mental health support with privacy and convenience. Appointments can be scheduled in advance, just like in-person care.
How does teleMentalHealth work ?
Just like most virtual medical visits, teleMentalHealth starts with a patient or their healthcare provider requesting a consultation. In emergency cases, it may be a nurse or physician in the emergency department, or on the med/surg floors. For outpatient care, it may be a healthcare provider in a physician’s office or clinic.
Once the consultation is requested, the mental health professional logs on to a videoconference with the patient, who is in a private location. This could be a room in the hospital, or in a physician’s office or clinic. It could even be in the patient’s home.
The teleMentalHealth professional establishes the purpose of the virtual medical consultation and evaluates the patient. Sessions are typically 45 minutes to an hour, similar to in-person care. At the end of the consultation, the mental health professional provides feedback to the patient on follow up care, as well as documents the visit. In the case of emergency telePsychiatry, the psychiatrist would provide documentation and feedback to the hospital staff for additional testing, treatment, and/or follow up care.
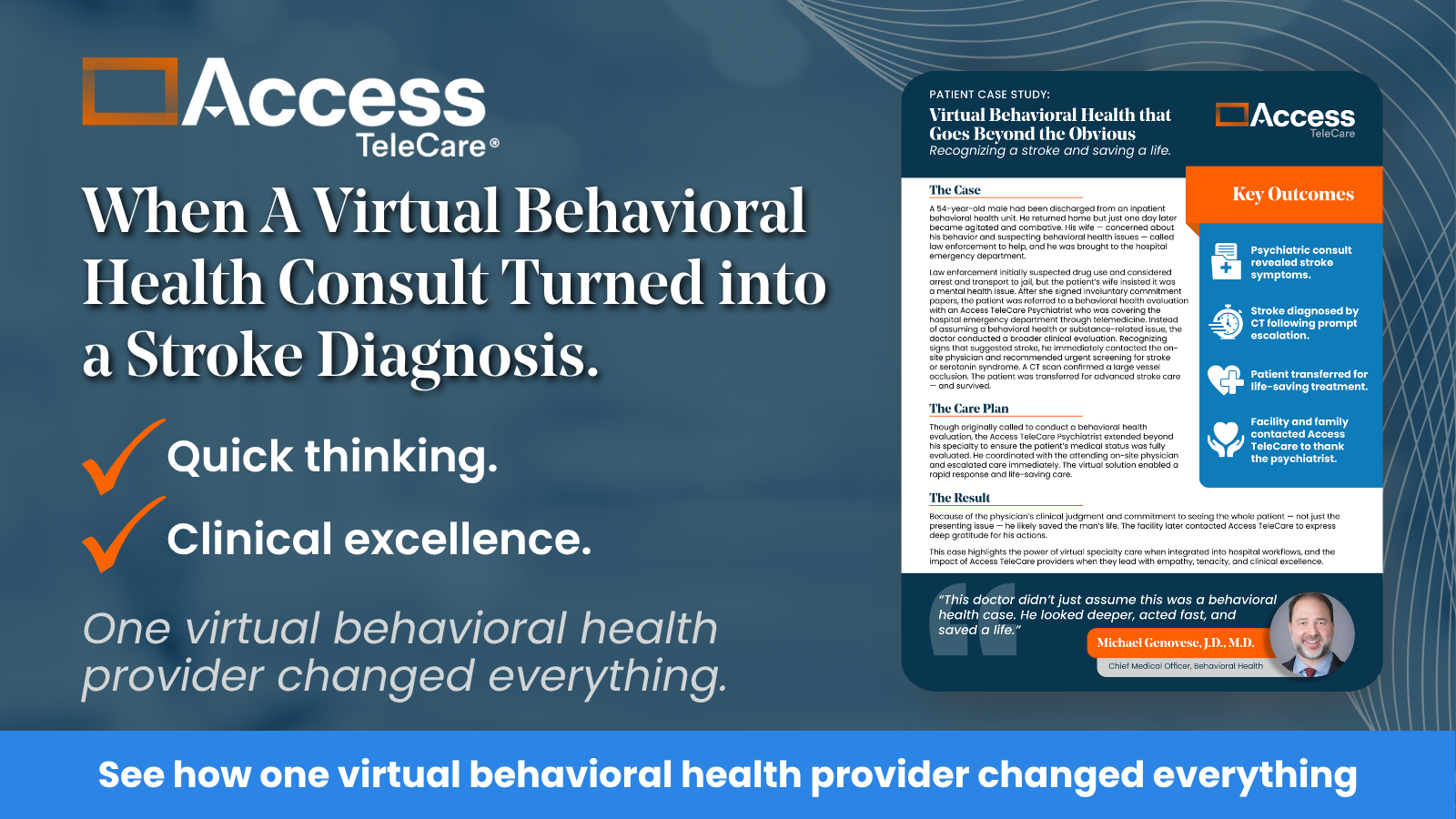
More From Access TeleCare
See behavioral health in action with the power of Access TeleCare and telemedicine.
What are the benefits of teleMentalHealth ?
- Emergency Departments: Remote psychiatrists can quickly consult with the patient and onsite staff for acute mental health emergencies. See also telePsychiatry.
- Inpatient: Hospitals without onsite psychiatrists can request consultations from specialists to address sudden changes to patients’ mental health status in the hospital for other treatments.
- Outpatient: Post-crisis mental health for those patients who are not an immediate threat to themselves or others; may have sought care in the emergency room and are now at home. In-person appointments can typically take weeks or months; these patients need help sooner in order to avoid a subsequent crisis.
- Physician Offices and Clinics: Primary care providers are often the first healthcare professionals to become aware of patient mental health issues. Having access to teleMental Health care in the same familiar office via a private video conferencing room means patient convenience and more comprehensive care.
- Schools: Using videoconferencing technology, mental health professionals can be available for students in crisis or for ongoing treatment
- Prisons: Most prisons do not have a psychiatrist or other mental health professional on-site. Mental health professionals can safely see inmates over a camera and eliminate the need for either party to travel. See also: Sandra Bland Act
- Substance Abuse Treatment Centers: Many substance abuse patients have underlying mental health issues; having a mental health professional available over video is part of a holistic treatment plan.
Expanding Mental Health Access With TeleMentalHealth
TeleMentalHealth is an efficient use of scarce mental health resources. With an increase in the number of patients with mental health and substance abuse issues, teleMentalHealth can help provide access to professionals quicker and more conveniently than in-person care.
Learn more about Access TeleCare’s virtual behavioral health services. Contact us today to discover how teleMentalHealth can enhance patient care and expand access to mental health specialists.