Rural hospitals are at the center of an urgent conversation today. Rising patient demand and acuity, constrained resources, and staffing shortages make it harder every year for rural hospitals to keep essential specialty services available. Telemedicine for rural health offers a proven solution; helping hospitals sustain services, support their teams, and ensure their communities get the care they need, close to home.
How Telemedicine Helps Rural Hospitals Improve Access
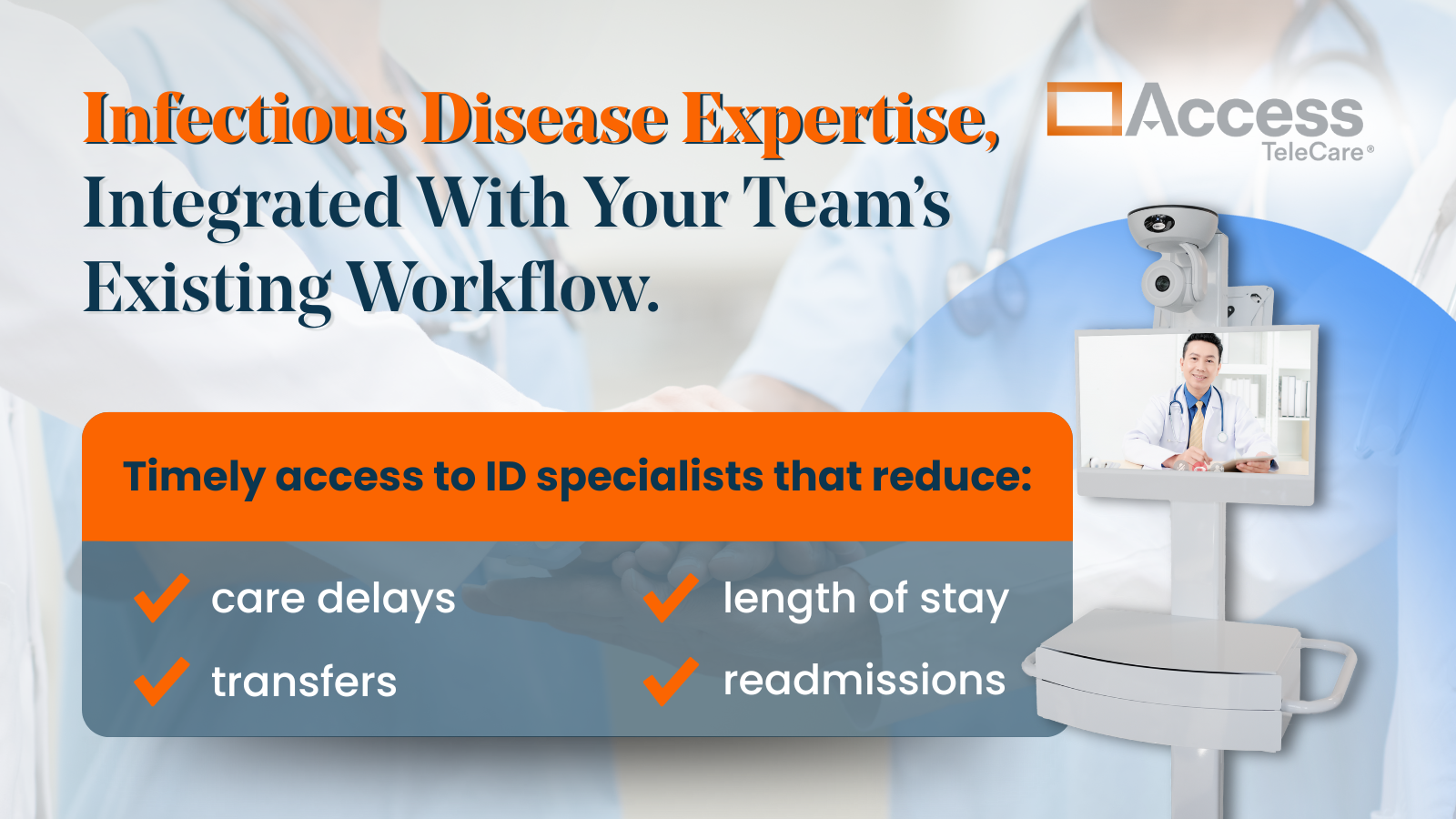
Rural hospitals experience challenges that their urban counterparts don’t. Recruiting and retaining specialists is often more difficult, and transfers can delay care and jeopardize outcomes. Telemedicine for rural hospitals changes this equation by connecting facilities to board-certified specialists in real time without the need for full-time on-site physicians.
Key benefits of telehealth for rural hospitals include:
-
Faster access to specialized care: teleNeurology, behavioral health, and other specialty consults are available 24/7, reducing delays in care.
-
Keeping care local: Patients stay closer to home, avoiding costly transfers.
-
Supporting local clinicians: Telemedicine expands the team, reducing burnout and providing backup when staffing gaps arise.
-
Improving hospital sustainability: Rural hospitals can keep service lines going, improving revenue stability, and strengthening community trust.
Benefits of Telehealth in Rural Areas for Patients and Hospitals
The impact of telemedicine in rural areas is more than convenience; it’s measurable improvement in outcomes and hospital performance. By embedding virtual specialists into existing workflows, rural hospitals can scale services that would otherwise be unavailable.
For patients, this means access to life-saving interventions like stroke care within the critical treatment window. For hospitals, it means the ability to deliver specialty services that attract and retain patients locally.
Telehealth for Rural Hospitals: A Sustainable Care Model
The traditional model of staffing every specialty with in-person clinicians simply isn’t feasible for most rural hospitals. Telemedicine provides a sustainable alternative, one that aligns with both patient needs and hospital operations.
By connecting to specialists virtually, rural hospitals can:
- Respond to emergencies faster.
- Maintain service lines even with physician shortages.
- Build long-term care capacity without overextending resources.
“Virtual specialty care isn’t just a stopgap, it’s a foundation for care delivery,” said Joshua DeTillio, CEO, Access TeleCare. “By combining best-in-class technology with clinical expertise, we’re giving rural hospitals a way to meet demand today and prepare for the future.”
The Future of Rural Health Is Virtual
As state leaders, hospital executives, and policymakers look for solutions to strengthen rural healthcare, telemedicine stands out as a proven, scalable option. It preserves access to care, stabilizes hospitals financially, and ensures that rural communities aren’t left behind.
For rural hospitals, the question isn’t whether to adopt telemedicine; it’s how quickly they can integrate it to safeguard services and secure the future of care in their communities.