Understanding TeleCardiology: How Virtual Cardiovascular Care Works
What is teleCardiology ?
TeleCardiology is the diagnosis and treatment of disorders of the heart, such as congenital heart defects, coronary artery disease, and heart failure by a remote clinician using technology like videoconferencing. It makes it possible for a cardiologist and patient to be in separate rooms, cities, states or even countries and still be connected face-to-face.
TeleCardiologists can work with onsite staff to help manage patients experiencing varying cardiac issues, such as arrhythmia, heart failure, and chest pain.
How does teleCardiology work in a hospital ?
When a patient with a cardiac condition arrives at the ED, they can expect to give blood for tests, get an IV, and undergo tests, such as an electrocardiogram (EKG). They will be monitored for abnormal heart rhythms. A cardiologist reviews the lab work and test results, then examines the patient, via a telemedicine cart. After discussion with the patient and onsite staff, the cardiologist makes recommendations for treatment, which may include medication, catheterization, or heart surgery.
Once a patient is admitted, cardiologists can continue to see them virtually, as well as use teleCardiology for follow up visits.
More From Access TeleCare
See teleCardiology in action with the power of Access TeleCare and telemedicine.
How teleCardiology can reduce transfers
Generally, in smaller hospitals, cardiac issues can often be the primary reason for transfer. Many of these patients only need a consultation to determine whether they can be retained and treated close to home, and avoid the disruption of transfer to a tertiary hospital. Additionally, community hospitals may also be in need of a solution for patients who do not require invasive treatment and procedures and can benefit from a teleCardiology consultation. TeleCardiology services, which operate 24/7, provide board certified expert cardiologists who can support hospitalists and internists, as well as Emergency Department physicians in the management of these patients.
What are the benefits of teleCardiology ?
Improved care for cardiac patients
- Increased access to specialists not otherwise locally available
- Faster response times to see patients during a cardiac event
- Reduced waiting times for conducting necessary procedures
Increased throughput in the ED
- Increased access allows for more efficient patient treatment
Higher patient and provider satisfaction
- Patients receive quality cardiac care in their local hospital instead of being transferred out of their community
- Providers who work the day shift can have relief on nights and weekends for better quality of life; this aids hospitals in keeping the cardiologists they have
Improved financial position
- Reduction of patient transfers
- Reduction of locum tenens and recruiting costs
- Increased revenue by retaining patients
- Reduced average length of stay (ALOS)
The impact of TeleCardiology on cardiovascular care and patient outcomes
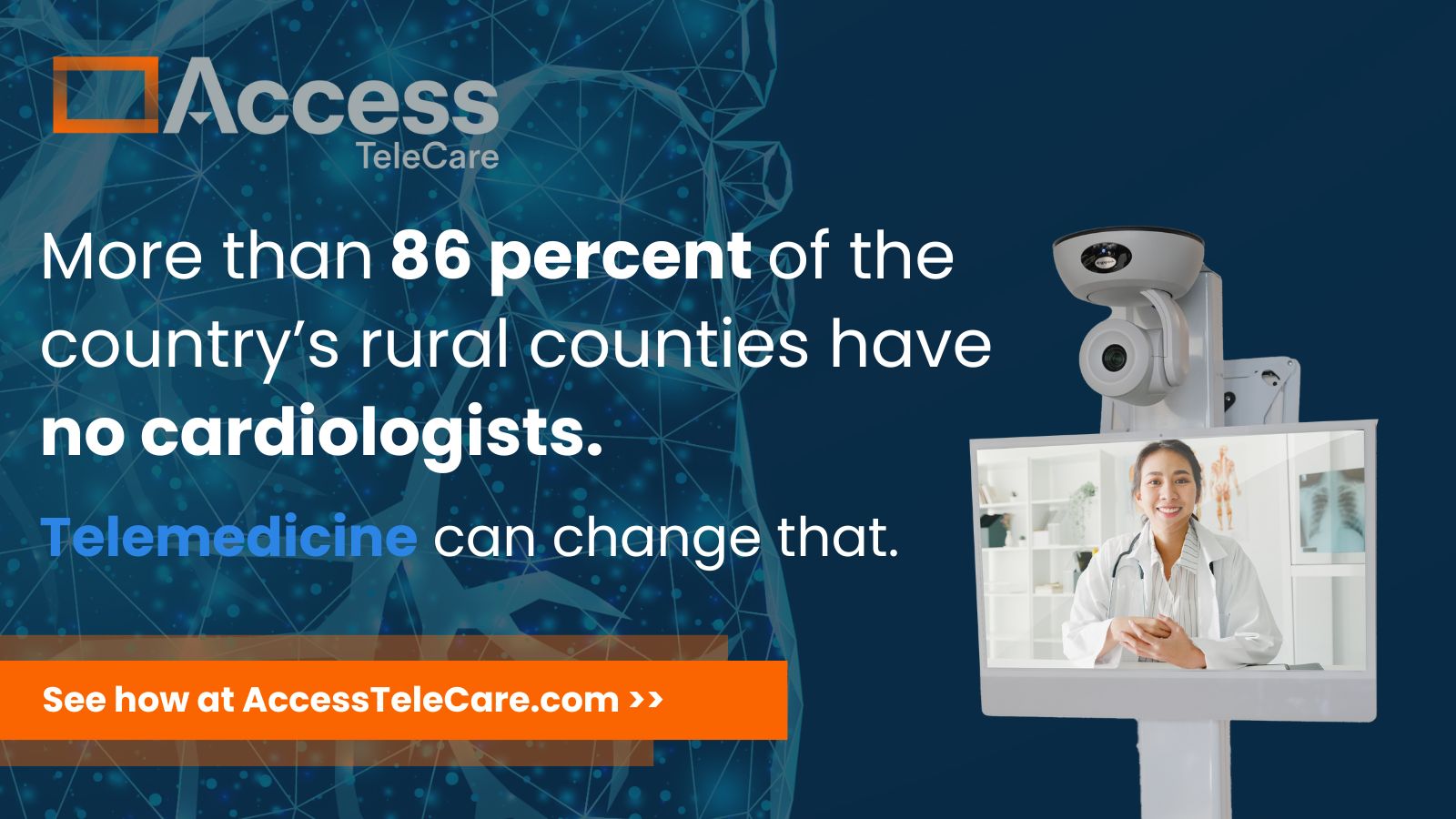
TeleCardiology is an efficient use of scarce clinical resources. With an aging population, an increase in the number of patients with cardiovascular disease, and a decrease in the number of cardiologists, teleCardiology can fill a gap for cardiac care. By using teleCardiology, hospitals can retain more patients and more revenue. Augmenting with teleCardiologists for nighttime or weekend coverage can provide their own physicians with a better quality of life.
Contact us today to learn how Access TeleCare’s TeleCardiology services can help your hospital provide expert cardiac care 24/7.